One Anastomosis Gastric Bypass
The Single Anastomosis Gastric Bypass (Omega Loop Gastric Bypass/Mini-gastric Bypass/Single-Anastomosis Bypass) has gained proponents throughout the world, particularly increasing in the past years in Europe and Asia. Several Studies have demonstrated that it is a rapid, safe and effective bariatric operation,
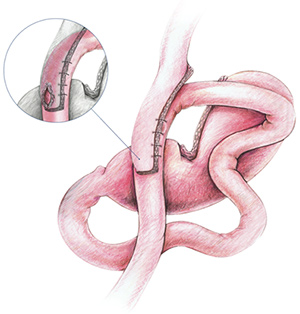
The operation consists of two components: First, a long and narrow – restrictive lesser-curvature gastric pouch; Second, a 200 cm jejunal bypass with a single antecolic gastro-jejunostomy (GJ) anastomosis, which leads to significant (fat-)malabsorption.
Single Anastomosis Gastric Bypass
Operation:
Creation of the Gastric Pouch
The lesser curvature of the stomach is identified at the level or just distal to the craw’s foot. Here, the lesser sac is entered and the stomach stapler-divided (not completely transsected) at a right angle to the lesser curve. An app. 36 Fr bougie is passed down by the anaesthetist, and the stomach is further stapler-divided upwards parallel to the lesser curvature, so creating a narrow, longitudinal gastric pouch. The fundus is explicitely not part of the pouch.The long and narrow shaped pouch is less prone to dilation because there is no outlet narrowing by a stoma or pylorus.
Creation of the 200-cm Malabsorptive Jejunal Bypass
The omentum is retracted from left to right to enable exact identification of the Duodeno-Jejunal junction (ligament of Treitz).
The small bowel is run to 200 cm distal to Treitz’ ligament and
then anastomosed antecolic end-to-side to the gastric pouch.
Some surgeons vary the length of the bypassed small bowel according to the BMI, with longer bypassed small bowel segements in superobese patients. Care must be taken to have at least 300cm of small bowel in the food stream to avoid an increased risk of side effects due to malabsorption.
To minimize possible bile reflux, some surgeons perform additional sutures between the afferent biliopancreatic limb and the gastric pouch. Clinicially relevant bile reflux is reported in the literature in the low one-digit percentage range and can be easily corrected by conversion to a Roux en Y gastric bypass or an entero-enterostomy.
Until today there is no evidence that the Single Anastomosis Gastric Bypass promotes the development of gastric- or esophageal cancer, although this question (due to the lack of long-term data) cannot be answered definitely.
The expected weight loss is at least comparable to the Roux en Y Gastric Bypass – or even better (range 30-40% Body Weight Loss). The same is true for the resolution of comorbidities, especially Diabetes.[4]
Patients after Single Anastomosis Gastric Bypass need (micronutrient) supplementation comparable to that after RYGB,additionally there is a higher risk for iron deficiency and deficiency for fat soluble vitamins.
Fat malabsorption may limit the quality of life in few patients especially after a high-fat diet due to bloating and steatorrhea.
The number of Single Anastomosis Gastric Bypasses performed worldwide is increasing steadily: This procedure has proven to be technically simple, safe and effective, resulting in permanent weight loss, being easily revisable by moving the anastomosis, and if ever necessary, reversable.
- Georgiadou, D., et al., Efficacy and safety of laparoscopic mini gastric bypass. A systematic review. Surg Obes Relat Dis, 2014. 10(5): p. 984-991.
- Lee, W.J., et al., Laparoscopic mini-gastric bypass: experience with tailored bypass limb according to body weight. Obes Surg, 2008. 18(3): p. 294-9.
- Garcia-Caballero, M. and M. Carbajo, One anastomosis gastric bypass: a simple, safe and efficient surgical procedure for treating morbid obesity. Nutr Hosp, 2004. 19(6): p. 372-5.
- Lee, W.J., et al., Laparoscopic Roux-en-Y Vs. mini-gastric bypass for the treatment of morbid obesity: a 10-year experience. Obes Surg, 2012. 22(12): p. 1827-34.
